Implementing the Safe Handling of Oral Anti-Cancer Drugs in Community Pharmacies

A Pan-Canadian Consensus Guideline
Authors: Dr. Kathy Vu1,2, Ms. Heather Logan3, Ms. Erika Brown3, Ms. Suzzette Oriasel2
Introduction
Community pharmacists will encounter more oral anti-cancer drugs (OACD) in their pharmacies. Approximately 46%1 to 60%2 of cancer drugs that are coming out of the oncology pipeline are oral agents. OACD are commonly used alone or in combination with intravenous (IV) systemic treatment as part of a regimen. These agents may also be referred to as take-home cancer drugs (THCD) as it allows the patient a more convenient and less invasive approach to cancer treatment at home. With the shift in the delivery of treatment to the community setting, there is concern regarding the management of occupational hazard risk associated with inadvertent exposure to these drugs in a community pharmacy setting.
Rationale for the guideline
Ontario has a decentralized dispensing model, therefore THCD may be filled at any community pharmacy in Ontario. While standards and guidelines have been developed to ensure safe dispensing and administration of IV chemotherapy, there are few published for OACD with specific considerations for dispensing in community pharmacies.3
Cancer Care Ontario (CCO) launched the Systemic Treatment Provincial Plan 2014 – 2019 which aims to improve the safety, quality, and accessibility of systemic treatment in Ontario. One of the priority areas is to ensure the safety and quality of THCD dispensed in community pharmacies. To address this priority focus, CCO collaborated with the Canadian Association of Provincial Cancer Agencies (CAPCA) and the Canadian Pharmacists Association (CPhA) to develop the Safe Handling of Oral Anticancer Drugs in Community Pharmacies: A Pan-Canadian Consensus Guideline to provide guidance around the safe dispensing and handling of oral anti-cancer drugs in low-volume settings unique to the community pharmacy setting.
The guideline was informed by existing evidence and through discussions with executive level community pharmacy leaders. Each recommendation was reviewed and revised through an iterative process to obtain consensus. It was also reviewed by more than 30 external organizations with mandates in patient or medication safety, occupational health and safety, transportation of hazardous drugs, and/or pharmacy practice. The whole process was guided by a group of experts with knowledge in medication and patient safety, community pharmacy practice, oncology pharmacy practice, health system design, as well as individuals who represent patients and their families (the “Task Force”). The guideline provided recommendations for each point of medication lifecycle where exposure to the drug can occur. It addressed manufacturer packaging and labelling, receiving and unpacking, storage, preparation and handling, verification and dispensing, disposal and waste management, spill protocols, personal protective equipment, training and education, staffing, and incident reporting.
The guideline is intended to supplement mandatory legislative standards. It complements existing legislation, regulation, and professional practice standards. When there is inconsistency or conflict between the recommendations, the mandatory or more restrictive requirements should take precedence.
The full published guideline is available at: https://www.cancercareontario.ca/sites/ccocancercare/files/guidelines/full/OACDs_in_Community_Pharmacy.pdf
Recommended Starting Points
It is expected that the full implementation of these guidelines will be challenging because of their complexity, the novelty with respect to established practice and the infrastructure needed to support their implementation. As part of the work of developing the recommendations, feedback on implementation timelines was requested from those responsible for change management (see Figure 3)
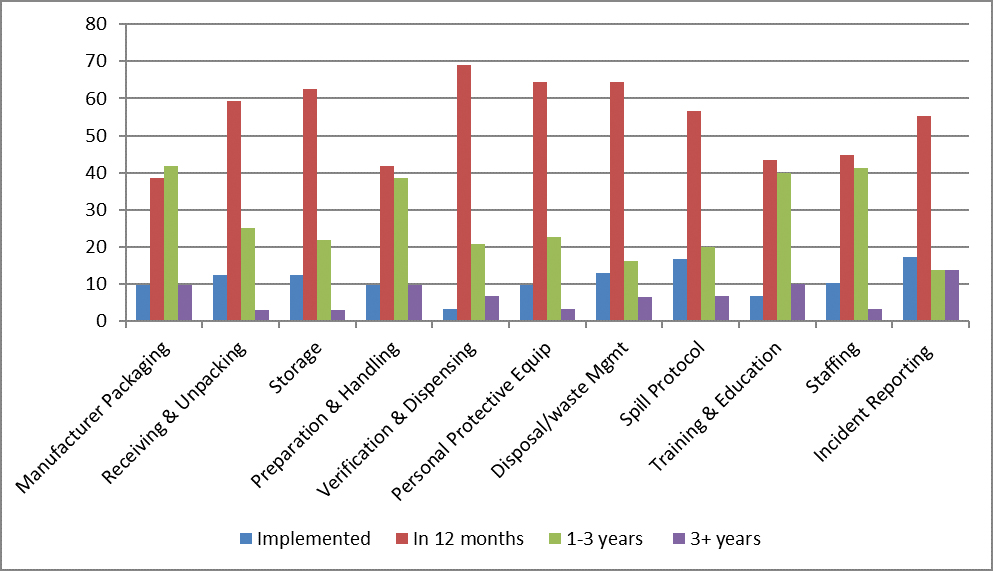
Figure 3: Expected Implementation by External Review Respondents (n=32)
To address the need to balance safety and feasibility of incorporating the recommendations into practice, the Task Force took a pragmatic approach and considered alternatives that minimize contamination and eliminate confusion to enhance adoption of the recommendations. An example is wearing two pairs of gloves when handling OACDs to eliminate confusion over the number of gloves and the associated task. In doing so, there is a risk of non-adherence to double gloving and potential inconsistencies with other guidelines. However, the Task Force felt that a consistent approach was important, thus the message is to wear gloves when handling OACD with less emphasis on the number of gloves.
We recommend that pharmacy staff, managers and owners review the guideline and have open discussions to understand the concerns and where to focus resources to implement the recommendations. We further suggest starting with the following, unless there are other priority areas identified.
A. Train staff
CCO collaborated with the Leslie Dan Faculty of Pharmacy at the University of Toronto, and the Canadian Association of Pharmacy Oncology (CAPhO) to develop the Oncology Program for Pharmacists: A Person-Centred Approach to Cancer Care for pharmacists in all practice settings. This two-part program (Essentials of Oncology and Advanced Oncology) aims to provide standardized education for pharmacists to ensure safe and high quality care to cancer patients and their caregivers. For more information, visit http://cpd.pharmacy.utoronto.ca/oncology.html.
Staff should be encouraged and given an opportunity to participate in continuing education programs as appropriate for their knowledge, skills, and job functions. We recommend that clinical verification of a THCD prescription should be done by a pharmacist with experience and training in cancer treatment. If such a pharmacist is not available onsite, it is important that another experienced and trained pharmacist is available for consultation. The use of a clinical checklist is highly recommended. Cancer Care Ontario developed a checklist that can be customized and adapted for the purpose of documentation (see https://www.cancercare.on.ca/common/pages/UserFile.aspx?fileId=362139).
Similarly, all staff who handle hazardous drugs should have training at the start of their job and routinely when job functions change or after a prolonged absence. Pharmacy managers should ensure that a trained backup staff is available for unpacking and dispensing of OACDs in case of absences.
B. Create a list of hazardous drugs encountered
in the pharmacy
Drugs that are considered hazardous to humans or animals are associated with one of the following characteristics: 1) carcinogenicity; 2) teratogenicity or other developmental toxicity; 3) genotoxicity; 4) reproductive toxicity; 5) organ toxicity at low doses; and 6) structure and toxicity profiles of new drugs that mimic existing drugs determined by the above criteria4. OACDs pose hazards through dermal absorption, inhalation, and ingestion via contaminated surfaces. Coated tablets or capsules that are solid and intact without modifications when administered to patients may pose less significant risk.4 However, uncoated tablets are at risk of forming dust when subjected to stress (e.g. when poured in and out of a container, and repeatedly counted), which can contaminate the workplace.4
While there is no single list of hazardous drugs that is accepted worldwide, the National Institute of Occupational Safety and Health (NIOSH) produces and updates a list periodically that can be used as a guide from which to develop a workplace or setting-specific hazardous drug list based on an inventory of the drugs handled and the potential for exposure. Guidance on how these workplace-specific lists should be developed is available through NIOSH at https://www.cdc.gov/niosh/topics/antineoplastic/pdf/hazardous-drugs-list_2016-161.pdf (link no longer available).
We suggest that the Designated Manager or a delegate and staff compile a list of hazardous drugs that require additional caution (e.g. segregated space or the use of personal protective equipment). This list should be posted in all areas of the pharmacy where there may be contact with OACD (e.g. receiving, storage, dispensing and disposal areas). The list should be reviewed annually at a minimum and with each new drug that enters the pharmacy. All OACD on this list should have a visible label to indicate that they require additional precaution (e.g. personal protective equipment).
C. Physically separate OACDs
It is best practice to have a separate room for receiving, unpacking of OACD shipments and storage where access is restricted to staff who have received appropriate training. However, since space may be limited within the community pharmacy setting, all activities involving OACD should (at minimum) be done in a designated, low-traffic area that is clearly marked off and labelled distinctly to indicate extra caution is required. We further recommend that storage of OACD in the dispensary be segregated from all other non-hazardous drugs. This will help to limit staff exposure, lower the risk of medication error through incorrect selection of medication, and provide a visual indication that special handling is required.
In addition to dedicating separate physical space for handling and storing OACD, it is also important to dedicate separate equipment to be used solely with hazardous drugs. This includes a dedicated counting tray and spatula as well as disposal containers for hazardous drugs only. Disposal containers should be rigid with a lid and clearly marked for hazardous drugs only. These containers should be made available where OACD are handled and disposed of by incineration by an appropriate company.
D. Evaluate available tools and current compounding practices
In some cases, the prescribed dose of an OACD is not commercially available and compounding is required. Class I Biological Safety Cabinet (BSC) is recommended for the compounding of non-sterile hazardous drugs. When a containment cabinet is not available for non-sterile compounding, consider other alternative tools and practices to minimize contamination to the work area and staff. Safe work practices while wearing personal protective equipment (PPE) in a low-traffic, designated area, along with the use of tools that minimize exposure may be sufficient. Examples include crushing tablets with mortar and splitting tablets inside an enclosed clear and re-sealable bag, wetting the tablet prior to crushing to minimize aerosolization, and using devices such as Dissolve-a-DoseTM containers.
When dispensing, the final packaging should prevent or minimize access and exposure to unintended individuals. Whenever possible, the medications should be dispensed in their original packaging, in containers with childproof lids (unless otherwise requested), and/or have additional packaging such as resealable plastic bags to contain inadvertent spills. OACDs should be dispensed in a ready-to-use formulation that reduces the need for cutting/crushing in order to eliminate/minimize patient/caregiver exposure.
E. Ensure availability of personal protective equipment (PPE)
While engineering and administrative controls are being considered for implementation and when other safety controls cannot be obtained, PPE is the last line of defense. Community pharmacies should have the following PPE available; ASTM standard D-6978-05 chemotherapy gloves, certified hazardous waste protective gowns, fitted respiratory protective masks (N95 or better), and protective eyewear. The following are recommended:
- Two (2) pairs of non-sterile gloves during all activities involving OACD (except transport, receiving and handling in final dosage form.)
- A gown when cleaning preparation areas (including containment cabinets), handling waste (including damaged packages and spills) and compounding if there is a risk of splash or spill (e.g. liquids).
- Respiratory protection mask when cleaning the containment cabinet or handling damaged packages and spills.
- Eye protection when cleaning preparation areas (including containment cabinets), compounding if there is a risk of splash or spills (e.g. liquids) and handling damaged packages and spills.
- Hair cover when cleaning the containment cabinet.
- Shoe cover when cleaning the containment cabinet and when handling damaged packages and spills.
Summary
The set of recommendations were made to be practical and introduce a reasonable approach that encourages a system-wide and gradual change in community pharmacy practice. However, it is not unexpected that the complete adoption of the above recommendations will be challenging, especially those vastly different to established practices and infrastructure.
Designated Managers are encouraged to assess their current practices, address possible barriers to implementation, and discuss ways in which the recommendations can be adopted. As oral anti-cancer drugs become more prevalent in community settings, pharmacies must be prepared to handle them safely.
References:
- Cancer Care Ontario. Quality Person-Centred Systemic Treatment in Ontario 2014-2019 Systemic Treatment Provincial Plan. Available from: https://www.cancercare.on.ca/common/pages/UserFile.aspx?fileId=325326
- Canadian Association of Provincial Cancer Agencies. Oral Cancer Drug Therapy Safe Use and Safe Handling Guidelines 2015. Available from: http://www.capca.ca/wp-content/uploads/En-Oral-Chemotherapy-Guideline-Final-11-May-2015.pdf
- Cancer Care Ontario. Think Tank: Enhancing the Delivery of Take-Home Cancer Therapies in Ontario. Available from: https://d3n8a8pro7vhmx.cloudfront.net/cancertainty/pages/34/attachments/original/1419012064/Think_Tank_Proceedings_Report_December_2014.pdf
- The National Institute for Occupational for Occupational Safety and Health. NIOSH List of Antineoplastic and Other Hazardous Drugs in Healthcare Settings, 2016. Available from: https://www.cdc.gov/niosh/topics/antineoplastic/pdf/hazardous-drugs-list_2016-161.pdf (link no longer available)
AUTHORS:
- Cancer Care Ontario, Toronto, Ontario, Canada,
- Leslie Dan Faculty of Pharmacy, University of Toronto, Ontario, Canada
- Canadian Association of Provincial Cancer Agencies (CAPCA), Toronto, Ontario, Canada
